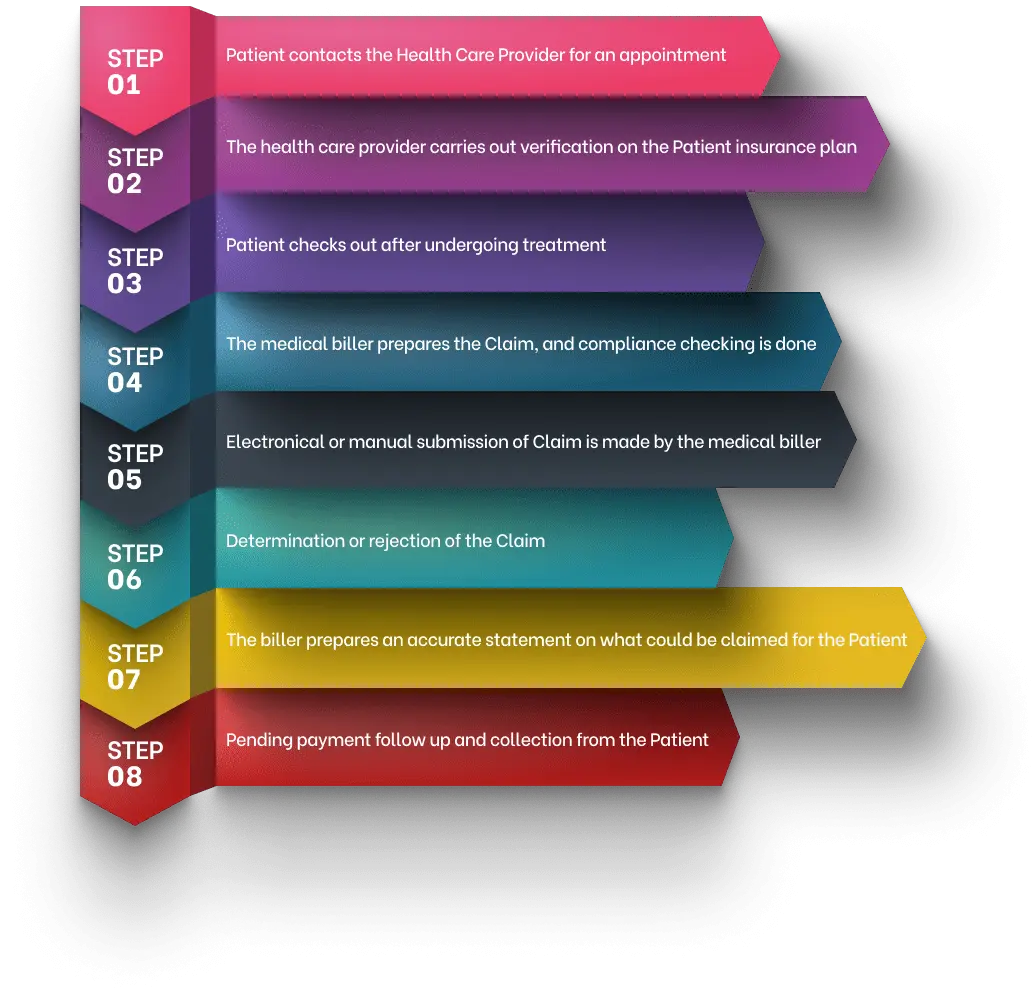
Step 1: Appoinment Scheduling - The patients' healthcare organization or clinic is contacted for patient appointment with the healthcare provider. Some clinics choose to schedule appointments using an advanced software application, whereas a few prefer to manually.
Step 2: Insurance Eligibility Verification - The most critical step in revenue cycle management is patient insurance eligibility verification. This step is paramount for the last bit of the procedure. The plan coverage and various benefits of the patients' medical expenses as stated in their insurance card must be critically verified by the provider or their assigned staff team.
Step 3: Medical Records Management - The provider needs to carry out certain medical procedures on the patient as per requirement. Following this, the medical records are passed over to the billing team by the provider. During this step, the patient checks out.
Step 4:Medical Billing - The medical billing team verifies the health records, and specific codes are denoted for the various medical procedures performed. The claim is prepared according to the conditions mentioned in the patients' insurance policy.
Step 5: Insurance Claim - After thoroughly verifying the provided data, the medical billing team submits the claim to the insurance networks. While a more significant number of payers accept electronic claims, a few groups still prefer to present the claims manually.
Step 6: Payer Contract Management - It takes a while as the insurance networks examine the submitted claims. Simultaneously, the medical billing team must follow up regularly with the payer's contract. The claim is further accepted, denied based on specific errors, or even rejected wholly based on the preciseness of the submitted claims. Being a medical biller, all that you need to be concerned about is that the details on the proposed claim are free of errors and complete.
Step 7: Payment Processing - As soon as a part of the claim is reimbursed by the insurance payer, the patient must make the balance payment. The medical billing team is responsible for preparing a comprehensive bill for the patient with the total insurance coverage and explaining carefully about the out-of-pocket expenses.
Step 8: Billing Collections - The final step is to collect the possible credit balances from the patient or insurance, and also refund the patient or payer appropriately for the over-payments received. According to the laws, there are specific clauses in balance billing the patient, such as the No Surprises Act. Staying updated with the current trends and recent changes effectively is highly recommended.
A revenue cycle management flowchart is a useful tool to help you manage your business. By creating a flowchart, you can see how your business is developing and where money is going. This will help you to make better decisions about where to allocate resources and budget.